

Lymphomas arising from the EAC are extremely rare. Complete surgical excision is the treatment of choice. Histologic examination is mandatory for the correct diagnosis, and high-resolution temporal bone computed tomography is of great help in delineating the tumor involvement. The differential diagnosis for EAC hemangiomas may include cholesteatoma with an aural polyp, arteriovenous malformation, granulation tissue, glomus tumor, and carcinoma. However, most patients do not show any symptoms, and are diagnosed incidentally because the size of the tumors is small, ranging from 5 mm to 3 cm in diameter. Patients with EAC hemangiomas may present with symptoms such as hearing loss, aural fullness, tinnitus, or bloody otorrhea. To the best of our knowledge, ours is the first reported case of a venous hemangioma in the EAC. Twenty-six cases with hemangioma arising from the EAC have been reported in the literature, and, in most of these cases, the histologic type was capillary or cavernous. Arteriovenous malformation, which is characterized by an interconnected complex of arterial and venous structures, can also be included as a category of hemangioma. Hemangioma is one of the most common soft tissue tumors, and can be classified into capillary, cavernous, and venous. No measurable remaining mass lesion was observed on follow-up CT 6 months after treatment. The patient was treated with local radiotherapy of 50.4 Gy, which reduced the size of the tumor dramatically ( Fig. Therefore, clinical staging was performed using brain magnetic resonance imaging, computed tomography of the abdomen and chest, whole-body positron emission tomography, and bone marrow biopsy, which revealed no other localization of the lymphoma. Immunohistochemical staining tests showed that the atypical lymphoma cells were positive for CD20, CD79a, BCL2, BCL6, and Mum-1, and negative for CD3 and CD10, thereby suggesting a diagnosis of DLBCL. Histopathological examination revealed diffuse proliferation of abnormally large lymphoid cells ( Fig. Under the clinical impression of a malignant soft-tissue tumor, we performed an incisional biopsy. High-resolution temporal bone computed tomography demonstrated an infiltrative, enhancing soft-tissue mass with complete obstruction of the left EAC and bony erosion of the inferior wall of the EAC moreover, the mass lesion extended to the left parotid space ( Fig. Conductive hearing loss with a 35-dB air-bone gap was noted on pure tone audiometry. 2A), which made the tympanic membrane invisible.
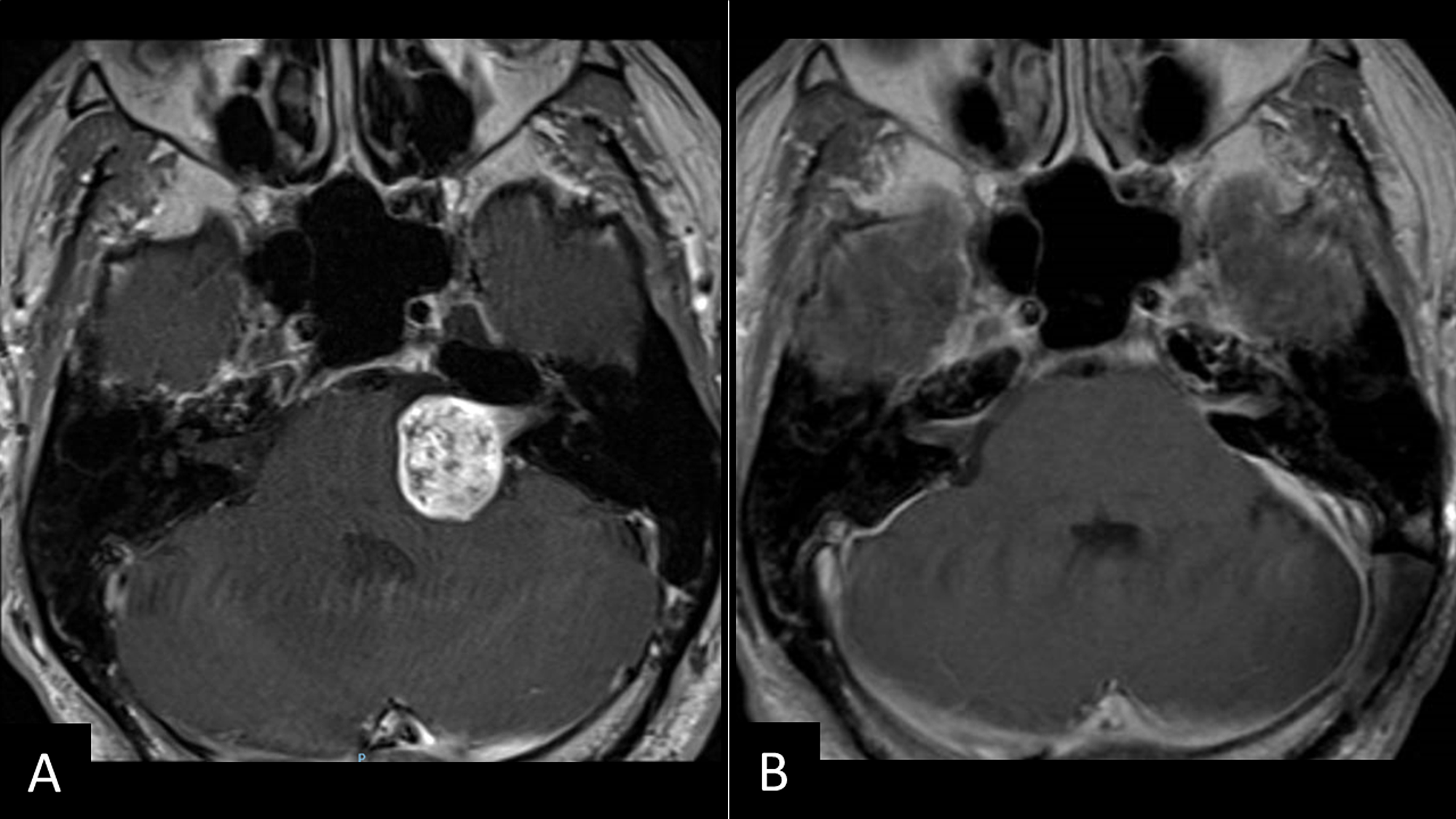
Otoendoscopic examination revealed a reddish polypoid mass obstructing the left EAC ( Fig. She did not report headache or dizziness, and had no previous history of ear disease, ear or brain trauma, otologic surgery, or lymphoproliferative disorder. She had visited another hospital before being referred to our clinic, and had undergone incisional biopsy that revealed a histologic diagnosis of a ruptured epidermal cyst. The patient had been experiencing ear fullness, hearing loss, otorrhea, and otalgia on the left side for 2 months. 3A).Ī 76-year-old woman was referred to our clinic with the left EAC mass lesion. After 16 months postoperatively, the patient has shown no evidence of recurrence ( Fig. Histopathological examination revealed a proliferation of thick-walled vessels that were variably dilated in the myxoid stroma ( Fig.
#Internal auditory canal cyst skin
The mass was completely removed, and a skin graft was not required. The mass originated from the superior wall of the EAC, and was confined within the EAC. We performed an excisional biopsy of the mass via the transcanal approach under a surgical microscope. No evidence of extension into the middle ear cavity was noted. High-resolution temporal bone computed tomography revealed a soft-tissue mass with mild enhancement without bony erosion or destruction in the right EAC ( Fig. Pure tone audiometry revealed conductive hearing loss with a 35-dB air-bone gap on the right side. The tympanic membrane was not visible because of the EAC mass lesion.
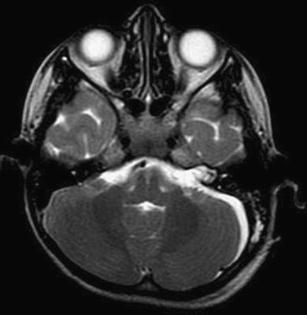
Otoendoscopic examination revealed a reddish mass obstructing the EAC ( Fig. She had no previous history of otorrhea, otologic surgery, or recent ear or brain trauma. The patient reported bleeding from the right ear after ear picking 2 weeks ago, and did not complain of otalgia, otorrhea, or dizziness. A 55-year-old woman visited our clinic with a symptom of slowly progressing hearing loss on the right side.


 0 kommentar(er)
0 kommentar(er)
